A study involving over 17-million people in England has revealed that certain factors can heighten one’s chances of dying from COVID-19. The study published to Nature is the largest of its kind, say the authors, and reveals interesting disparities along racial groupings.
Scientists tracked the health of 17 278 392 adults over the course of three months. Over this time period, 10 926 died of COVID-19 or complications related to the virus. The study confirms what is already known about the vulnerable, saying that those at higher risk of dying are older people, men, racial and ethnic minorities and of course, those with underlying health conditions.
“The overall cumulative incidence of death 90 days after study start was less than 0.01% in those aged 18-39 years, rising to 0.67% and 0.44% in men and women respectively aged ≥80 years ,” reads the study. “Increasing age was strongly associated with risk, with those more than 80 years having more than 20-fold increased risk than 50-59 year olds.”
“Men had higher risk than women. These findings are consistent with patterns observed in smaller studies worldwide and in the UK,” the study continues.
“All non-white ethnic groups had higher risk than those with white ethnicity. Non-white ethnicity has previously been found to be associated with increased COVID-19 infection and poor outcomes. Our findings show that only a small part of the excess risk is explained by higher prevalence of medical problems such as cardiovascular disease or diabetes among BME people, or higher deprivation.”
Medical conditions like severe asthma, diabetes and obesity were also shown to contribute to poor outcomes.
While most of this is already known, the statistics on race and ethnicity are especially compelling as they suggest minority groups are disproportionately burdened by the virus. This leads to further questions on how social and structural inequalities affect the spread and experience of COVID-19.
According to the New York Times, federal data reveals that Black and Latino people across various age groups and areas in America are being infected at a much higher rate. They are three times more likely to become infected than white residents in America, and nearly twice as likely to die. Dr Uchechi Mitchell, a public health expert at the University of Illinois at Chicago, says this shows that the disparities among COVID-19 cases and deaths are linked to structural racism.
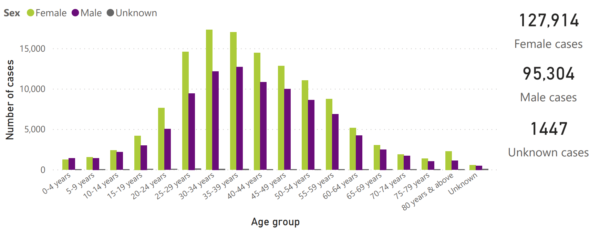
Interestingly, according to the National Institute for Communicable Diseases (NICD), laboratory data from the public and private sectors in South Africa as of July 8 reveal that 127 914 confirmed COVID-19 cases are women and 95 304 are men, while 1447 are unknown.
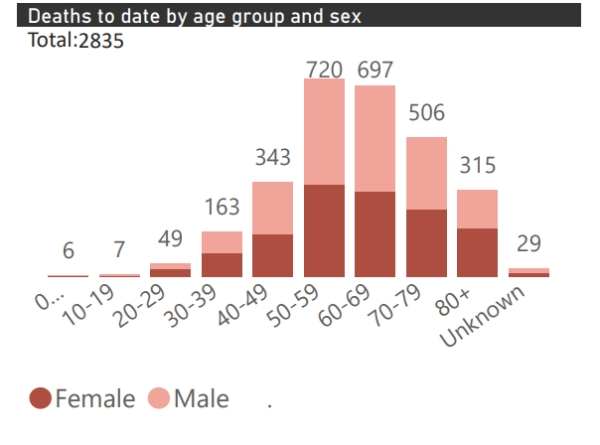
Most of the deaths, however, are men. Of the 2 835 deaths recorded as of Wednesday, July 8 the majority are male and fall within the 50-59 and 6o-69 age groups.
This report on age and sex only presents data collected using clinical information from admitted patients at selected hospitals, so these stats are not reflective of the entire country. Not all hospitals currently participate in the report and new facilities continue to enroll.
Breakdowns on infections and deaths based on racial or ethnic groupings in the country are not currently available.
“We have demonstrated – for the first time – that only a small part of the substantially increased risks of COVID-19 related death among non-white groups and among people living in more deprived areas can be attributed to existing disease. Improved strategies to protect people in these groups are urgently needed,” concludes the study.
“These might include specific consideration of BME groups in shielding guidelines and work-place policies. Subsequent studies are needed to investigate the interplay of additional factors we were unable to explore, including employment, access to personal protective equipment and related risk of exposure to infection and household density.”

